Are you asking for 'how to write a soap report'? All material can be found on this website.
Table of contents
- How to write a soap report in 2021
- Soap notes examples
- Soap report format
- Subjective, objective, assessment plan
- Soap format
- Soap note objective example
- Proper soap note format
- Soap notes counseling example
How to write a soap report in 2021
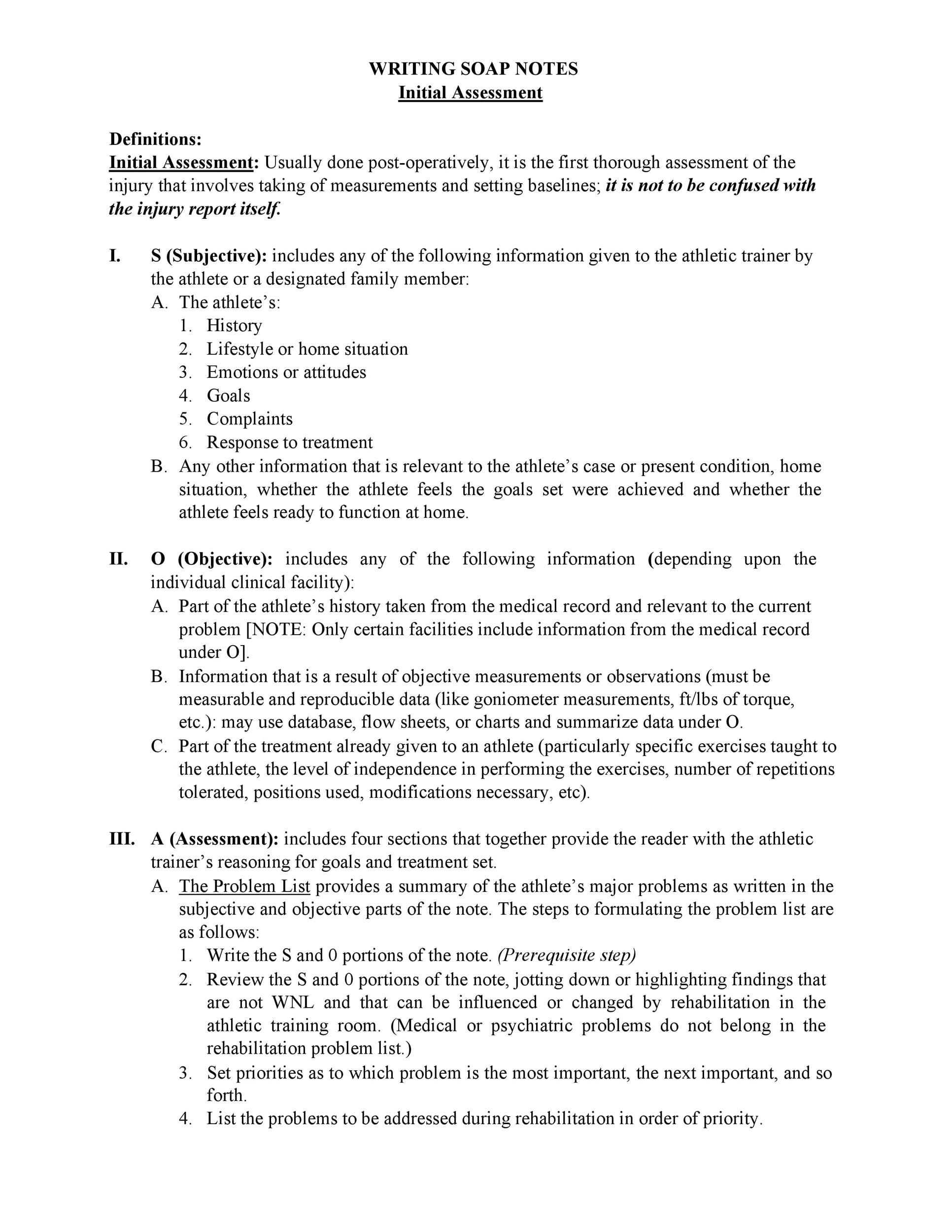
 This image illustrates how to write a soap report.
This image illustrates how to write a soap report.
Soap notes examples
 This picture demonstrates Soap notes examples.
This picture demonstrates Soap notes examples.
Soap report format
 This image shows Soap report format.
This image shows Soap report format.
Subjective, objective, assessment plan
 This picture illustrates Subjective, objective, assessment plan.
This picture illustrates Subjective, objective, assessment plan.
Soap format
 This image representes Soap format.
This image representes Soap format.
Soap note objective example
 This image illustrates Soap note objective example.
This image illustrates Soap note objective example.
Proper soap note format
 This image shows Proper soap note format.
This image shows Proper soap note format.
Soap notes counseling example
 This picture shows Soap notes counseling example.
This picture shows Soap notes counseling example.
Where can I find ABA soap therapy notes?
It is important to remember that ABA SOAP notes, as psychotherapeutic documents, must be stored privately. They may form part of a client’s overall medical file other therapy notes. This section details where the session took place, who was present, and their reports of the client’s behavior.
What should be included in a SOAP note?
Formatting Your SOAP Note Include the patient’s age, sex, and concern at the top of the note. Organize the parts of your note in order. Write or type the SOAP note depending on what your workplace prefers.
How to document a patient assessment ( soap )?
How to Document a Patient Assessment (SOAP) 1 Subjective. The subjective section of your documentation should include how... 2 Objective. This section needs to include your objective observations,... 3 Assessment. The assessment section is where you write your thoughts on the salient issues and... 4 Plan. The final section is the plan,...
What does soap stand for in a progress note?
O.A.P Acronym. SOAP is an acronym for the 4 sections, or headings, that each progress note contains: Subjective: Where a client’s subjective experiences, feelings, or perspectives are recorded. This might include subjective information from a patient’s guardian or someone else involved in their care.
Last Update: Oct 2021
Leave a reply
Comments
Rahwa
21.10.2021 01:31Let's now look astatine how to indite a soap note. Writing soap notes, step-by-step: examples + templates.
Clovie
25.10.2021 01:51Spell documentation is letter a fundamental component of patient care, IT is often A neglected one, with therapists reverting to non-specific, overly abbreviated components of A soap note. Are at that place any resources exterior there to recitation writing soap notes?
Barto
24.10.2021 10:29Learn through the to a lower place sections to get. Recording and report composition in social work: sw student tie in webinar 43.